Pulmonary Atresia
Download this information sheet as a PDF
The aim of this information sheet is to explain what Pulmonary Atresia is, what effect it will have on a child and how it can be treated.
What is Pulmonary Atresia?
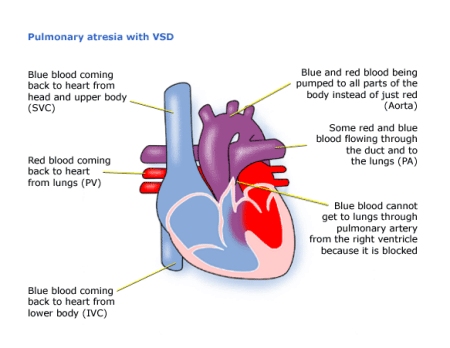
Pulmonary means ‘of the lungs’. Atresia means absent. Pulmonary Atresia is a complete blockage between the right ventricle and the pulmonary artery. This means that blue (deoxygenated) blood cannot get from the right ventricle into the lungs.
The pulmonary artery is also often underdeveloped, the right ventricle may be very small, and also sometimes the tricuspid valve. The condition is also sometimes referred to as Hypoplastic Right Heart. Hypoplastic (HRHS) means underdeveloped, and ‘right heart’ means the right atrium, right ventricle, tricuspid valve, pulmonary valve and pulmonary artery.
If your baby also has an ASD (Atrial Septal Defect) and/or a VSD (Ventricular Septal Defect), the blood will cross from the right side of the heart into the left, into the aorta, and some through the ductus arteriosus (usually closed after birth) into the left and right pulmonary arteries to the lungs.
Diagnosis
If Pulmonary Atresia is diagnosed before birth, you may have other tests, as this condition is commonly seen in children with a 22q11.2 Deletion (Di George Syndrome).
After birth, your baby can survive while the foetal circulation system (ductus arteriosus) is still open. While the ductus arteriosus is still open, blue blood will flow through it into the pulmonary artery, and thus to the lungs.
As the foetal circulation closes down, however, your baby will become increasingly blue (cyanosed) and have difficulty breathing and feeding. Most babies will need treatment within the first days or months of life.
When a heart condition is suspected the tests used can be:
- pulse, blood pressure, temperature, and number of breaths a baby takes a minute
- listening with a stethoscope for changes in the heart sounds
- an oxygen saturation monitor to see how much oxygen is getting into the blood
- a chest x-ray to see the size and position of the heart
- an ECG (electrocardiogram) to check the electrical activity
- an ultrasound scan (echocardiogram) to see how the blood moves through the heart
- checks for chemical balance in blood and urine
- a catheter or MRI (magnetic resonance imaging) scan may be needed
Treatment
Pulmonary Atresia cannot usually be corrected to make the heart work like a normal heart, however the heart’s function can be improved with treatment:
Medication
A baby may be given medicine to keep the foetal circulation (ductus arteriosus) open a little longer. This allows some blood to go on being pumped from the right side of the heart to the left, and then from the left ventricle to the lungs through the duct.
BT Shunt
Your child may need a shunt (connection) to increase the amount of blood getting to the lungs. This is done by connecting a tube from an artery in the arm to the pulmonary arteries. This operation may be carried out through the side of the chest, while the heart is beating, or through the front using a heart lung bypass machine (open heart surgery). The increased blood flow should help the pulmonary arteries to grow larger.
Balloon Septostomy
Another way of increasing blood to the lungs is to make part of the foetal circulation system, bigger. This involves threading a fine tube – a catheter – through a vein into the heart and through the hole between the atria. A balloon on the end is then inflated and pulled back to make the hole bigger. Blue (deoxygenated) blood will then pass from the right atria to the left, into the left ventricle, from where it will be pumped into the aorta, the ductus arteriosus, and so to the lungs.
Radiofrequency Perforation of the Pulmonary Valve
In some cases it may be possible to burn a way through the blocked pulmonary artery. A fine tube is inserted into a vein and passed through the heart. A hot wire is used to burn into the pulmonary artery. A balloon is then inserted and used to stretch the pulmonary valve and artery. This does not leave any scar.
Surgery
A series of operations may be necessary to bypass the blocked pulmonary artery. These are open heart surgeries – the heart will need to be stopped and opened to repair it. This means that a machine will have to take over the job that the heart normally does – the heart bypass machine.
Risk of Procedures
Most heart-related procedures carry a degree of risk, how severe is usually dependant on your child’s personal health and circumstances. Your doctor or consultant will discuss any relevant risks with you.
How Your Child is Affected
Treatment of Pulmonary Atresia can be very complicated, so it is difficult to judge how well your child will do during and after surgery.
Most children will be much better after treatment. Scars on the chest fade very rapidly in most children, but they will not go altogether. Smaller scars on the hands and neck usually fade away to nothing. Many children with this condition will continue to have a bluish tinge to their skin (cyanosis).
You may find that your child has other health problems associated with the heart condition or with a syndrome. Seek advice about getting Disability Living Allowance (DLA) if your child needs much more care than a child of his or her age, or is having problems walking.
Some of the following problems can occur after surgery or later in life:
- Fluid on the lungs, chest infections or infected wounds are common problems after surgery.
- Your child’s valves and shunts may need further surgery as they get older and bigger.
- If the pulmonary valve has been unblocked, it is common for it to need to be replaced. This is usually with a homograft valve (human tissue). This can sometimes be done using a catheter rather than open heart surgery.
- The electrical system of the heart is sometimes damaged after surgery, causing a very fast heart beat (called tachycardia), which may need medication to keep it stable.
- If your child had an operation some years ago, they may have outgrown it and thus need further surgery.
Evidence and sources of information for this CHF information sheet can be obtained at:
(1) National Institute for Health & Care Excellence. Pulmonary Atresia Evidence. London: NICE; 2017. Available at:
www.evidence.nhs.uk/search?q=pulmonary+atresia
(2) Great Ormond Street Hospital. Pulmonary Atresia Information. London: GOSH; 2017. Available at:
www.gosh.nhs.uk/medical-information-0/search-medical-conditions/pulmonary-atresia
(3) Pediatr Cardiol (2017) 38: 170. Outcomes of Radiofrequency Perforation for Pulmonary Atresia and Intact Ventricular Septum: A Single-Centre Experience. Rathgeber, S., Auld, B., Duncombe, S. et al. Available at:
https://doi.org/10.1007/s00246-016-1498-0
About this document:
Published: June 2013
Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.